Leg Length Discrepancy – A Critical Factor to a Successful Hip Replacement
In this post we would like to highlight the importance of the role that leg length discrepancy (LLD) plays in a successful total hip replacement. Most people go throughout the majority of their lives not ever thinking about the possibility that their legs are not 100% even in length. In fact, only about 10% of the population has an exactly equal leg length, whereas 90% of the population has a discrepancy of less than 1 cm. Again, the majority of these people will experience little to no limitations due to this slight difference. For patients undergoing a total hip arthroplasty (THA), LLD is a much more common occurrence, but with acute care and advances in technology, can be drastically reduced.
Studies have reported the incidence rates of LLD following total hip arthroplasty range from 1% to 50% and the average discrepancy ranging from 3 to 17 mm. While the joint pain caused by arthritis is solved, a LLD of just a few millimeters can cause long term issues such as lower back pain, a limp, potential revision surgery, and other functional limitations, resulting in an unsatisfactory outcome. In one study, new onset of lower back pain following a total hip replacement was reported in 11% of patients. Generally speaking, a LLD of greater than 10 mm is considered clinically unacceptable, however, it happens in up to 32% of THAs.
So, what is being done to minimize this common pitfall with total hip replacements? Accurate preoperative planning is the only way to help prevent potentially significant leg length discrepancies. There are several prominent ways that orthopedic surgeons template their hip replacements with the most dominant still being 2D radiograph (x-ray) templating. Unfortunately, this is one of the least reliable methods for accurately attaining an equal lower leg lower limb length. In one study, an evaluation of this templating technique led to the need to change the plan during surgery in 50% of the cases. Another drawback of this method is that it is extremely difficult to accurately predict implant size where, in one study, the correct implant size was predicted in only 60% of cases.
Why then is this method of hip templating the standard when studies show that there is a high percentage of inaccuracies? It has simply been the standard for decades. The process of taking x-rays and integrating them into patient charts for use in preoperative templating is well established in nearly all medical settings. The process is cheaper and faster than CT or MRI based imaging platforms, which also may require specialized software to perform the preoperative templating.
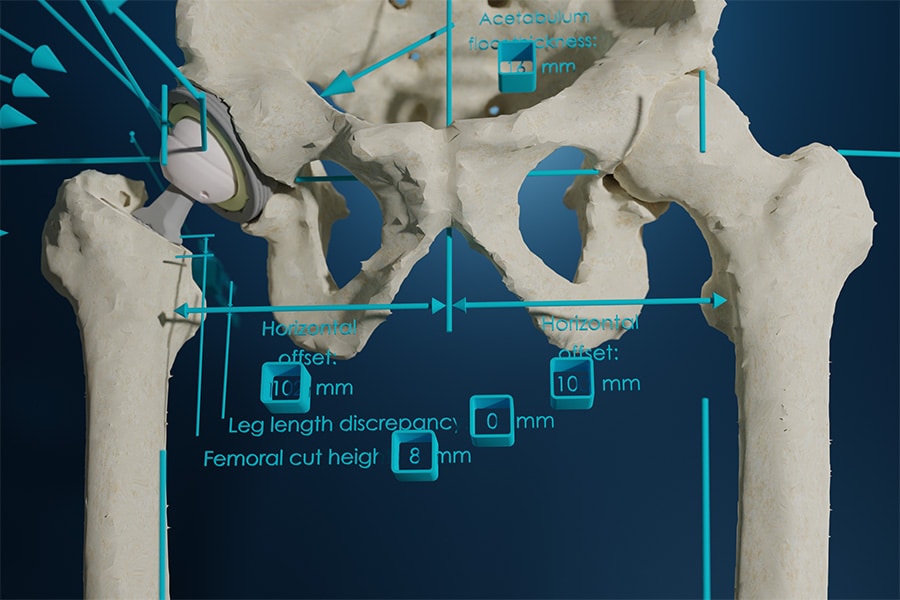
The more accurate option is 3D CT templating. In a meta-analyses there were six studies comparing 2D and 3D templating methods, in which all six found 3D templating to be more accurate with three of those studies reporting a statistically significant difference. There was a higher degree of accuracy in attaining a more equal leg length as well as implant sizing and positioning. This is one of Kinomatic’s core principles: to provide the most accurate preoperative plans possible. This is also why Kinomatic only uses CT imaging for their modeling; there is just no better representation of human anatomy than a 3D model.
LLD can be caused by multiple factors, both preoperatively and intraoperatively and remains a major factor in patient dissatisfaction following THA. Studies widely favor the accuracy of 3D templating over 2D templating, yet there are still few studies to support statistically significant long-term improvements. Joint replacements are meant to last 20-30 years. Functional outcomes are not as good following revision surgery to correct any malalignments or LLDs. So, when considering a joint replacement surgery, don’t you think it’s worth it to seek out the most accurate procedure for the best outcome possible?
To learn more about Kinomatic’s approach to delivering accurate joint replacement surgeries, click here.